🗞️ This week, fresh research shines a light on new therapeutic angles, quality-of-life challenges, and innovative clinical trials—all at a time when understanding lingering COVID effects is more urgent than ever. There is a lot of spotlight this week on ME/CFS, which is refreshing, especially because it feels like there has not been enough research we could highlight in previous issues.
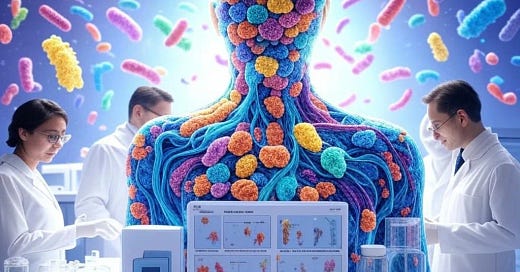
🗞️ **Article of the week: This week's article of the week is titled "The potential therapeutic approaches targeting gut health in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a narrative review," published in the Journal of Translational Medicine. The review explores the connection between gut health, microbiota composition, and therapeutic interventions for individuals suffering from ME/CFS. It highlights the significant impact gut dysbiosis has on symptom severity and overall health in affected patients.
Key findings from the review include:
"Notable changes in the gut microbiota diversity and composition in ME/CFS patients, contributing to systemic inflammation and worsening cognitive and physical impairments."
The review underscores the necessity of a “multidisciplinary approach,” acknowledging that “current research lacks comprehensive insights into how gut health might aid ME/CFS treatment,” which could pave the way for innovative therapies aimed at improving patient outcomes.**
Research
Article: The potential therapeutic approaches targeting gut health in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a narrative review | Journal of Translational Medicine | Full Text
Research suggests gut microbiome changes may play a role in ME/CFS symptoms and treatment
🗞️ Definitions
Dysbiosis: An imbalance in gut microbiota that may contribute to inflammation and neuropsychiatric symptoms.
Gut-Brain Axis: The communication system between the gut microbiome and the brain, affecting physical and mental health.
🗞️ Summary
Significant alterations in gut microbiota diversity and composition in ME/CFS patients may exacerbate systemic inflammation and cognitive impairments.
Interventions targeting the gut microbiome, including probiotics, prebiotics, and dietary changes, show potential as therapeutic strategies for ME/CFS.
There is evidence linking dysbiosis, gut permeability, and cognitive symptoms, highlighting the need for a multi-faceted approach to treatment.
Longitudinal studies and standardized protocols in assessing gut health in ME/CFS patients are necessary for innovative therapies.
🗞️ Stats/trends
The review synthesized results from various studies over two decades, emphasizing qualitative and quantitative analyses of gut microbiota and inflammatory markers in ME/CFS patients.
Notable microbial changes were reported, though a consistent dysbiotic pattern was not identified across studies.
Interventions explored included probiotics, prebiotics, dietary modifications, and fecal microbiota transplantation, showing varied patient responses.
Article: Heart Rate Variability Modulation Through Slow-Paced Breathing in Health Care Workers with Long COVID: A Case-Control Study | The American Journal of Medicine
Slow-Paced Breathing May Improve Long COVID Symptoms
🗞️ Definitions
Slow-paced breathing: The voluntary slowing down of respiratory frequency, linked to a range of positive mental and physical health outcomes.
Heart rate variability (HRV): Changes in the time intervals between consecutive heartbeats.
Photoplethysmography (PPG): A method for measuring HRV.
🗞️ Summary
Disruption in vagal activity can account for disturbances present in Long COVID.
This intervention study compared HRV parameters in Long COVID vs non-COVID and post COVID health care workers prior to and during the enhancement of cardiovagal tone obtained using slow-paced breathing.
Both vagally mediated (vmHRV) time and frequency domains parameters increased consistently among groups during slow-paced breathing. In the Long COVID group, mean heart rate also was found to be increased.
The study found no change in the PPG-assessed cardiac autonomic system in Long COVID at rest compared with controls, but signs of vascular reactivity dysfunction were present. Slow breathing was able to attenuate this finding, suggesting that slow breathing exercises may help restore vascular impairment and reduce long-term cardiovascular risk.
Repeated sessions may act as an effective non pharmacological, no-cost, self-administered intervention to help improve this condition. Further long-term follow-up is needed to evaluate the effectiveness of the protocol used.
Article: Cerebrospinal fluid immune phenotyping reveals distinct immunotypes of myalgic encephalomyelitis/chronic fatigue syndrome | The Journal of Immunology | Oxford Academic
Study Reveals Distinct Immune Profiles in ME/CFS Patients, Highlighting Diversity in Disease Experience
🗞️ Definition
Pathogen Seroreactivity: The presence of antibodies against specific pathogens, indicating prior exposure or infection.
🗞️ Summary
The study identified two distinct immunotypes of ME/CFS based on cerebrospinal fluid (CSF) analysis, revealing important differences in disease profiles among patients.
While clinical presentations were similar, distinct pathogen exposures and inflammatory profiles were observed between patient clusters.
Unsupervised hierarchical clustering of CSF samples revealed two clusters correlating with different matrix metalloproteinase (MMP) profiles, underscoring immune heterogeneity within ME/CFS.
A significant proportion of patients experienced higher pain and fatigue compared to matched healthy controls, suggesting substantial quality of life impairment.
Investigating immune profiles in ME/CFS may lead to potential biomarker discovery and targeted therapies for more effective management.
🗞️ stats/trends
The study involved 81 participants—40 diagnosed with ME/CFS and 41 matched healthy controls.
Samples from 79 participants (39 ME/CFS and 40 controls) were collected for analysis between November 2021 and June 2022.
CSF samples from 34 ME/CFS patients showcased distinct immunophenotypic signatures among participant clusters.
🗞️ Counterpoints
The study lacks control CSF samples, so there is no comparison group for the ME/CFS immunotypes..
The modest sample size may limit the generalizability of the results, highlighting the need for larger cohorts in future studies.
Article: Association of Pre‐COVID Fitness With Post‐COVID Fitness and Long COVID in the Cooper Center Longitudinal Cohort Study | Journal of the American Heart Association
Lower pre-COVID fitness levels linked to higher risk of long COVID symptoms, study finds
🗞️ Definition
Cardiorespiratory Fitness (CRF): A measure of the body's ability to supply oxygen to muscles during sustained physical activity, often quantified in metabolic equivalents (METs).
🗞️ Summary
The study highlights a significant association between pre-COVID fitness levels and the development of long COVID symptoms, indicating that lower cardiorespiratory fitness may predispose individuals to persistent symptoms post-infection.
Individuals who developed long COVID had a baseline mean cardiorespiratory fitness (CRF) of 10.0 METs compared to 11.1 METs for those who recovered, revealing a substantial fitness difference prior to infection.
Following COVID infection, those with long COVID demonstrated persistently lower CRF levels, with mean fitness metrics declining to 9.8 METs, indicating a lack of recovery compared to other groups.
The findings suggest that pre-COVID fitness, measured from 2017 to 2023, may predict long COVID development, emphasizing the importance of maintaining physical health.
🗞️ Stats/trends
The research included 4,005 participants, aged 20 to 74, with their cardiorespiratory fitness assessed before and after COVID infection.
Among the 1,666 individuals who reported COVID, only 80 (4.8%) met the criteria for long COVID, emphasizing that most reported symptom resolution within three weeks.
Pre-COVID, the average CRF for pre pandemic participants was 11.3 METs, while uninfected participants averaged 10.7 METs.
🗞️ Counterpoints
While the study offers valuable insights, it is important to consider the observational nature of the research and potential biases associated with a cohort limited to health-conscious individuals.
Article: Self-reported health, neuropsychological tests and biomarkers in fully recovered COVID-19 patients vs patients with post-COVID cognitive symptoms: A pilot study | PLOS One
Study Reveals Lower Quality of Life in Post-COVID Patients Despite No Cognitive Test Differences
🗞️ Definitions
Neuroplasticity: The brain's ability to adapt and reorganize itself by forming new neural connections, essential for recovery from cognitive deficits.
Biomarkers: Biological indicators measured to assess health conditions, including inflammation and neuroplasticity factors.
🗞️ Summary
The study compares two groups of post-COVID patients—those experiencing cognitive symptoms (long COVID) and fully recovered individuals—focusing on cognitive functioning, self-reported health, quality of life, and relevant biomarkers.
Patients with long COVID reported significantly lower quality of life, physical health, emotional functioning, and psychological well-being compared to controls, despite no significant differences in overall cognitive test performance.
The long COVID group scored significantly lower on a measure of letter fluency, indicating potential verbal processing difficulties (p < 0.05).
Serum levels of nerve growth factor (NGF), a key biomarker of neuroplasticity, were significantly lower in the long COVID group, suggesting impaired brain plasticity.
🗞️ Stats/trends
The study involved 17 participants: 10 with cognitive symptoms associated with long COVID and 7 fully recovered individuals serving as controls.
The long COVID group had notably lower scores on letter fluency tests (raw score: 26.80 vs. 38.00; p = 0.043).
Long COVID patients exhibited significantly higher rates of IL-10 levels above the median compared to controls (p = 0.015).
Article: Living With Long COVID: Everyday Experiences, Health Information Barriers and Patients' Quality of Life | Health Expectations
Long COVID Patients Face Significant Healthcare Barriers, Leading to Emotional Distress and Isolation
🗞️ Definitions
Quality of Life (QoL): A multi-dimensional concept encompassing physical health, mental and emotional well-being, social relationships, and overall life satisfaction.
Health Information Barriers: Challenges patients face in accessing and understanding health information, often influenced by stigma and misinformation.
🗞️ Summary
The study reveals significant barriers faced by Long COVID patients in accessing healthcare and reliable information, resulting in emotional distress and reduced quality of life.
Participants reported chronic pain and post-exertion fatigue, with 56.5% unemployed or on sick leave, highlighting the economic impact of the condition.
Access to healthcare was fragmented, often leading to long waiting times and inadequate follow-up care, which caused feelings of abandonment and frustration.
Many patients preferred online resources for information over healthcare providers, due to perceived unreliability from professionals.
Emotional and social challenges were prevalent, with stigma affecting patients' sense of isolation and overall well-being.
🗞️ Stats/trends
A total of 23 semi-structured interviews were conducted with participants diagnosed with Long COVID in Spain, ranging from 19 to 63 years old (mean age 45.3, SD = 8.7).
Financial instability was reported by 56.5% of participants, emphasizing the economic burden associated with Long COVID.
Article: Meta-transcriptomics Reveals Dysbiosis of Respiratory Microbiome in Older Adults with Long COVID | Research
Study Finds Altered Respiratory Microbiome in Older Adults May Contribute to Long COVID Symptoms
🗞️ Definitions
Meta-transcriptomics: A high-throughput sequencing technique analyzing RNA transcripts in microbial communities, providing insights into active functions and interactions.
Dysbiosis: An imbalance in the microbiome's composition, which can negatively affect health, especially related to respiratory diseases.
Alpha Diversity: A metric assessing species variety in a sample, indicating microbial ecosystem stability.
🗞️ Summary
The research reveals significant dysbiosis in the respiratory microbiome of older adults with Long COVID, characterized by a decrease in beneficial bacteria.
Meta-transcriptomic analysis indicated that Long COVID patients showed impaired respiratory microbial functions, contributing to ongoing pulmonary complications.
Alpha diversity of the respiratory microbiome was significantly lower in Long COVID patients than in healthy controls, suggesting a less stable ecosystem.
Specific bacterial genera, including Lactobacillus and Bacteroides, were markedly reduced in Long COVID patients, correlating with increased inflammatory markers.
Restoring a balanced respiratory microbiome could potentially mitigate Long COVID symptoms and improve recovery outcomes.
🗞️ Stats/trends
The study analyzed respiratory samples from 150 older adults with Long COVID and 50 matched healthy controls.
The alpha diversity index was significantly lower in Long COVID patients (Shannon index: 2.10 ± 0.56) compared to controls (3.25 ± 0.72; P < 0.001).
Key beneficial genera like Lactobacillus were present in only 25% of Long COVID patients, compared to 70% in healthy subjects (P = 0.001).
Article: Evaluating the Causal Role of Genetically Inferred Immune Cells and Inflammatory Cytokines on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | Biomedicines
Study Links Elevated Inflammatory Cytokines to Symptoms of ME/CFS, Suggesting New Treatment Paths
🗞️ Definitions
Genetically Inferred Immune Cells: Immune cell populations derived from genetic data that may provide insights into responses and susceptibility to diseases, including ME/CFS.
Inflammatory Cytokines: Signaling molecules that mediate and regulate immunity and inflammation; their dysregulation is associated with chronic illnesses.
🗞️ Summary
The research establishes a causal relationship between elevated inflammatory cytokines and the prevalence of ME/CFS symptoms, emphasizing immune dysregulation.
Genetically inferred immune cell profiles indicated a significant association with ME/CFS, suggesting a hereditary component influencing disease susceptibility.
Patients exhibited significantly higher concentrations of pro-inflammatory cytokines compared to healthy controls, correlating with the severity of fatigue and pain symptoms.
Causal inference methods revealed that specific immune cell types can predict the likelihood of developing ME/CFS, marking a potential breakthrough in understanding the disease’s etiology.
The study suggests that targeting inflammatory pathways may offer new avenues for therapeutic intervention in managing ME/CFS symptoms.
🗞️ Stats/trends
The analysis included 150 participants, with 75 diagnosed with ME/CFS and 75 healthy controls.
Cytokine levels showed a statistically significant increase, with IL-6 at 45 pg/mL and TNF-α at 30 pg/mL in the ME/CFS group compared to 15 pg/mL and 10 pg/mL in controls (P < 0.001).
The proportion of genetically inferred immune cells categorized as activated T cells was 60% in the ME/CFS group versus 30% in the control group (P = 0.002).
🗞️ Counterpoints
Despite promising findings, the study's reliance on genetic associations may not fully encompass environmental factors contributing to ME/CFS.
Article: Health-related quality of life, physical and mental capacity at one year follow up of COVID-19 ICU patients: A prospective cohort study | Journal of Patient-Reported Outcomes | Full Text
Study Reveals High Prevalence of Long-Term Health Issues Among COVID-19 ICU Survivors After One Year
🗞️ Definitions
Health-Related Quality of Life (HRQoL): A multi-dimensional concept that includes subjective evaluations of both positive and negative aspects of life, particularly those affected by health status.
Post Intensive Care Syndrome (PICS): A collection of physical, cognitive, and mental health impairments that persist in patients after discharge from intensive care.
🗞️ Summary
Among 41 COVID-19 ICU survivors, a staggering 93% met the criteria for Post Intensive Care Syndrome (PICS) at the one-year mark, highlighting a significant burden of long-term health issues.
At the 6-month follow-up, patients reported profound fatigue, anxiety, and respiratory impairments, resulting in a 60% reduction in health-related quality of life compared to an age-adjusted normal population.
Cognitive testing revealed significant impairments, with 47% of participants using the Montreal Cognitive Assessment (MoCA) and 24% using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS).
Improvements in health-related quality of life at 6 months were not sustained at the 12-month follow-up, indicating ongoing physical and mental health limitations.
The results underscore the need for targeted rehabilitation interventions to address the complex needs of COVID-19 survivors, who continue to battle debilitating symptoms.
🗞️ Stats/trends
The study followed 41 adult COVID-19 patients discharged from ICUs in Sweden over a one-year period after their hospitalization between March and August 2020.
Fatigue was reported by all patients, with 100% scoring pathologically in the Multimodal Fatigue Inventory.
A 60% decrease in overall HRQoL was recorded at 2 months post-discharge, with only marginal improvement by the 6-month mark.
Article: Investigating the profile of patients with idiopathic inflammatory myopathies in the post-COVID-19 period | Microbiology Spectrum
COVID-19 Associated with Increased Cardiac Complications in Patients with Inflammatory Muscle Disorders
🗞️ Definitions
Idiopathic Inflammatory Myopathies (IIMs): A group of autoimmune diseases characterized by muscle inflammation and weakness.
Echocardiography: A diagnostic imaging technique used to visualize the heart's structure and function through ultrasound waves.
🗞️ Summary
This study reveals significant clinical changes in patients with idiopathic inflammatory myopathies (IIMs) following a COVID-19 infection, emphasizing cardiac complications.
The incidence of cardiac injury was 77.19% in the prior COVID-19 (PC) group compared to 63.64% in the no prior COVID-19 (NPC) group, suggesting COVID-19 may exacerbate IIMs.
Clinical manifestations like palpitations and increased heart disease activity scores were noted among IIM patients with a history of COVID-19.
Echocardiography demonstrated altered cardiac structure and function in the PC cohort, highlighting the long-term consequences of SARS-CoV-2 on heart health.
🗞️ Stats/trends
A total of 292 IIM patients were analyzed, with 171 having a history of COVID-19 and 121 without.
Cardiac injury was found in 77.19% of patients with prior COVID-19 compared to 63.64% without a history (P = 0.016).
The prevalence of palpitations was significantly higher in the PC group (21.05%) than in the NPC group (10.74%) (P = 0.031).
Article: People with Long COVID and ME/CFS Exhibit Similarly Impaired Dexterity and Bimanual Coordination: A Case-Case-Control Study - The American Journal of Medicine
Long COVID Patients Show Similar Motor Impairments to ME/CFS, Despite Shorter Illness Duration
🗞️ Definitions
Dexterity: Skill in performing tasks, especially with the hands, measurable through tests like the Purdue pegboard test.
Bimanual Coordination: Using both hands simultaneously for tasks, crucial for daily activities.
🗞️ Summary
Individuals with long COVID exhibit dexterity and bimanual coordination impairments similar to those seen in ME/CFS, despite a significantly shorter illness duration.
Performance scores on the Purdue pegboard test were comparable for both groups, indicating severe effects on fine motor skills.
The average duration of long COVID was approximately 16 months compared to 16 years for ME/CFS.
Impairments in dexterity and bimanual coordination contribute to increased disability, highlighting the need for targeted rehabilitation strategies.
There is an urgent necessity for healthcare interventions to improve dexterity and coordination in both populations, affecting daily living and employment.
🗞️ Stats/trends
The study involved 61 participants: 21 with long COVID, 20 with ME/CFS, and 20 healthy controls.
The Purdue pegboard test revealed similar dexterity levels between long COVID and ME/CFS patients.
Average age for long COVID participants was 47 ± 10 years, while ME/CFS participants averaged 50 ± 10 years.
Statistical analysis showed significant impairments in both groups compared to healthy controls, indicating substantial disability.
Article: Lessons Learned in Implementing a Multidisciplinary Long COVID Clinic - The American Journal of Medicine
Miami VA's Long COVID Clinic Demonstrates Success with Comprehensive, Multidisciplinary Treatment Approaches
🗞️ Definitions
Dysautonomia: A disorder with abnormal autonomic nervous system function, leading to symptoms like postural tachycardia or orthostatic hypotension.
Antinuclear Antibodies (ANA): Autoantibodies often associated with autoimmune diseases, present in various chronic conditions, including Long COVID.
🗞️ Summary
The establishment of a Long COVID Clinic at Miami VA emphasizes a multidisciplinary approach to diagnosing and treating complex symptoms.
Initial screenings showed that 85% of patients reported significant fatigue, with dyspnea (70%) and joint pain (73%) also common.
The clinic's whole health model integrates disciplines such as cardiology, neurology, and rehabilitation, resulting in improved patient outcomes.
Autonomic dysfunction was found in up to 50% of patients tested, highlighting the need for targeted interventions.
The model's integration of behavioral and pharmaceutical treatments proved more effective than isolated approaches, indicating a comprehensive therapeutic plan is essential.
🗞️ Stats/trends
The LCC began its pilot in 2020, assessing approximately 385 Long COVID patients during the study.
Data indicated that 50% of patients undergoing the NASA Lean Test experienced postural tachycardia or orthostatic hypotension.
Article: Excess Weight is associated with neurological and neuropsychiatric symptoms in post-COVID-19 condition: A systematic review and meta-analysis | PLOS One
Review shows excess weight associated with neuro symptoms in long COVID
🗞️ Summary
Of the 10,122 abstracts screened, 18 studies (n = 139,091 adults) were included. These studies included 79,050 subjects with excess weight vs 57,926 normal-weight subjects; there were 30,694 subjects with obesity vs 107,612 non-obese study subjects. Study authors assessed the risk ratios (RRs) and odds ratios (ORs) for the EW group.
The presence of excess weight in post-COVID condition (PCC) was significantly associated with persistent depression (RR = 1.21), headache (OR = 1.23), memory issues (RR = 1.43), sleep disturbance (RR = 1.31), and vertigo (RR = 1.21).
Obesity was significantly associated with persistent headache (OR = 1.45), numbness (RR = 1.61), smell disorder (OR = 1.16), taste disorder (OR = 1.22), and vertigo (RR = 1.44).
Excess weight, including overweight and obesity, is associated with experiencing neuro-symptoms related to PCC. Individuals with these conditions urgently need enhanced personalized care management.
Article: The PAX LC Trial: A Decentralized, Phase 2, Randomized, Double-Blind Study of Nirmatrelvir/Ritonavir Compared with Placebo/Ritonavir for Long COVID - The American Journal of Medicine [STUDY DESIGN]
Study Examines Nirmatrelvir/Ritonavir's Potential Benefits for Treating Long COVID Symptoms in Adults
🗞️ Definitions
Decentralized Trial: A clinical trial design allowing for remote participant engagement and data collection, improving access and reducing burden.
Nirmatrelvir/Ritonavir: An antiviral medication combination used to treat COVID-19 by inhibiting viral replication.
PROMIS-29: A standardized patient-reported outcome measure assessing multiple health domains focused on long COVID effects.
🗞️ Summary
The PAX LC trial investigates the efficacy and safety of nirmatrelvir/ritonavir in treating long COVID using a decentralized design for enhanced participant engagement.
The study involves 100 symptomatic adults in the contiguous United States, comparing outcomes between those receiving nirmatrelvir/ritonavir and placebo/ritonavir.
Primary endpoints focus on changes in the PROMIS-29 Physical Health Summary Score from baseline to Day 28, measuring treatment impact comprehensively.
Innovative methodologies include remote recruitment and digital diaries to streamline participant data collection and monitor health status effectively.
Secondary endpoints will evaluate cognitive function, symptom severity, and healthcare utilization.
🗞️ Stats/trends
The trial encompasses 100 participants, randomized into two groups (1:1) to receive either nirmatrelvir/ritonavir or placebo/ritonavir over 15 days.
Participants will complete daily digital diary entries to document compliance and any new or worsening symptoms.
Primary analysis will occur after all participants complete assessments on Day 28, with subsequent evaluations over 90 days.
Safety information will be monitored continuously, with daily reports on potential adverse events.
Media
Update from the field: Low dose Naltrexone for Treatment of long COVID | MN Department of Health Long Covid Guiding Council
Low Dose Naltrexone for Long COVID: A Review
🗞️ Summary
This update, published by the MN Department of Health in a series for clinicians, summarizes emerging evidence on low dose naltrexone (LDN) as a treatment option for patients with Long COVID.
Experts in Long COVID have taken an interest in LDN based on reported experiences by patients and a relevant mechanism of action.
A literature search on the use of LDN to treat long COVID was conducted through July 2024, yielding five published observational studies. Four were cross-sectional or cohort observational studies. One study was a pre-post LDN intervention study.
Among the notable findings, low dose naltrexone appears to be safe, and for some patients it may be effective at relieving long COVID symptoms. More rigorous studies, including randomized controlled trials, are needed to provide conclusive evidence of the beneficial effects of LDN.
For more detail on prescribing practices, see reference guide at: LDN Research Trust - The Low Dose Naltrexone Charity (https://ldnresearchtrust.org/2024_LDN_Guides)
🗞️ My Take (Amy)
Even though this update is targeted at clinicians, patients could bring it to their healthcare providers as helpful information if they were interested in starting on low dose naltrexone.
Article: Patients react to Trump’s closure of the long-COVID office: ‘I am horrified to think about care becoming less accessible’
🗞️ Summary
The closure of the Office of Long COVID Research and Practice has raised concerns about reduced access to vital care and research support.
Activists warn that existing healthcare gaps for long COVID patients could widen significantly due to the government's lack of commitment.
Patients fear that vulnerable populations will be disproportionately affected by systemic failures in access to care.
Real experiences highlight bureaucratic barriers, prolonged wait times for care, and inadequate medical knowledge surrounding long COVID treatment. Interviewees stress the need for increased awareness, research, and solidarity within the disability community to navigate challenges posed by long COVID.
🗞️ Stats/trends
An estimated 23 million people in the U.S. are affected by long COVID, underscoring the urgent need for comprehensive healthcare strategies.
The abrupt closure of the OLC has been criticized for exacerbating existing challenges faced by individuals seeking long COVID care.
Many patients report significant delays in accessing long COVID clinics, with wait times extending over a year for specialized care.
Article: BioVie Enrolls First Patient in ADDRESS-LC Clinical Trial
BioVie Inc. Begins Clinical Trial of Bezisterim to Treat Cognitive Symptoms of Long COVID
🗞️ Definitions
ADDRESS-LC Trial: A Phase 2 clinical trial evaluating the efficacy and safety of bezisterim for treating neurological symptoms related to long COVID.
Bezisterim: A novel anti-inflammatory compound under investigation for its potential to alleviate neuroinflammation and associated symptoms in conditions like long COVID.
🗞️ Summary
BioVie Inc. has enrolled its first patient in the ADDRESS-LC clinical trial to assess the anti-inflammatory candidate bezisterim for neurological symptoms related to long COVID.
Bezisterim is designed to modulate inflammatory pathways contributing to neuroinflammation, a key factor in cognitive impairments seen in long COVID patients.
The Phase 2 ADDRESS-LC trial is a randomized, placebo-controlled study, funded by the U.S. Department of Defense, targeting adults with cognitive impairment and fatigue due to long COVID.
Article: ‘I’m still battling this’: Endeavor Health recruiting patients for long-COVID studies
Ongoing Clinical Trials at Endeavor Health Explore Treatment Options for Long COVID Symptoms
🗞️ Definitions
Clinical Trials: Research studies evaluating the safety and efficacy of new treatments for long COVID.
Viral Persistence: When remnants of the virus remain in the body at low levels, potentially contributing to prolonged symptoms.
Exercise Intolerance: Undue fatigue or adverse effects during physical activity, often a symptom of long COVID.
🗞️ Summary
Endeavor Health is actively recruiting patients for three ongoing clinical trials aimed at understanding and treating long COVID.
Long COVID can manifest as over 200 different symptoms, including brain fog, fatigue, and cardiopulmonary issues.
Dr. Nirav Shah highlighted the role of viral persistence and autoimmune responses in long-term symptoms following COVID-19.
Ongoing trials at Endeavor Health focus on various aspects of long COVID, such as exercise intolerance and sleep disturbances.
Patients like Diane Patterson, battling long COVID for three years, emphasize the importance of clinical trials for finding effective treatments.
Article: Expert reveals the symptoms of Covid in 2025 - and how long infection now lasts | The Independent
🗞️ Definitions
Anosmia: A loss of smell, often reported during infections, particularly with certain variants of the virus.
Hybrid Immunity: Immunity from both vaccination and natural infection, providing enhanced protection against viruses.
🗞️ Summary
In 2025, COVID-19 remains a health concern, especially for vulnerable populations, despite most infections now resulting in mild illness.
A recent study involving healthcare workers showed a decline in the persistence of symptoms after subsequent COVID infections.
Anosmia continues to be reported with newer variants, although less frequently than with the original strains.
Vaccination is one of the most effective means to prevent severe COVID-19 illness and reduce the risk of long COVID.
As of early 2025, vaccination against COVID-19 has significantly reduced the risk of hospitalization and death among the general population.
Article: Genetic breakthroughs could point pharma to a long COVID drug | PharmaVoice
🗞️ Summary
Researchers are identifying specific genetic signatures associated with long COVID, potentially guiding targeted treatments for affected patients.
The findings from the U.K.'s LOCOME study may offer insights into the mechanisms of long COVID, linking genetic factors to clinical symptoms such as fatigue and cognitive impairment.
The hope is that these genetic clues will lead to viable treatments for long COVID within the next 12 to 18 months, filling a gap left by previous clinical trials that have largely failed.
Understanding gene interactions related to long COVID could also benefit patients with chronic fatigue syndrome, illustrating overlapping pathophysiological features. PrecisionLife's work suggests that a cheek swab test for genetic risk assessment might eventually help personalize treatment plans for long COVID and associated syndromes.




***FYI-Under the Media section: the article on Naltrexone might come in handy for people to show to their providers, who might be skeptical of trying it for them.